Abstract

INTRODUCTION: Asciminib is the first BCR-ABL1 inhibitor that potently inhibits kinase activity of the BCR-ABL1 oncoprotein by Specifically Targeting the ABL Myristoyl Pocket (STAMP). The primary analysis from ASCEMBL, a randomized, phase 3 trial, demonstrated that asciminib has superior efficacy and a better safety and tolerability profile than bosutinib (BOS) in patients (pts) with chronic myeloid leukemia in chronic phase (CML-CP) after ≥2 prior ATP-binding tyrosine kinase inhibitors (TKIs). The major molecular response (MMR) rate at wk 24 was 25.5% with asciminib vs 13.2% with BOS; the difference in MMR rates, after adjusting for major cytogenetic response status at baseline, was 12.2% (95% CI, 2.19-22.30; 2-sided P=.029). Grade ≥3 adverse events (AEs) were reported in 50.6% and 60.5% of pts receiving asciminib and BOS, respectively, and AEs leading to discontinuation in 5.8% and 21.1%, respectively. After a median follow-up of 19.2 months (or 7.5 months' additional follow-up since the primary analysis), we report updated efficacy and safety results from ASCEMBL.
METHODS: Adults with CML-CP treated with ≥2 prior TKIs were randomized 2:1 to asciminib 40 mg twice daily (BID) or BOS 500 mg once daily (QD). Eligible pts must have experienced treatment failure (lack of efficacy) per 2013 European LeukemiaNet recommendations for second-line TKI therapy or intolerance of the most recent TKI at screening. Pts intolerant of their most recent TKI were eligible only if they had BCR-ABL1 on the International Scale >0.1% at screening. Pts with known BOS-resistant T315I or V299L mutations were ineligible. The cutoff date for the current analysis was January 6, 2021.
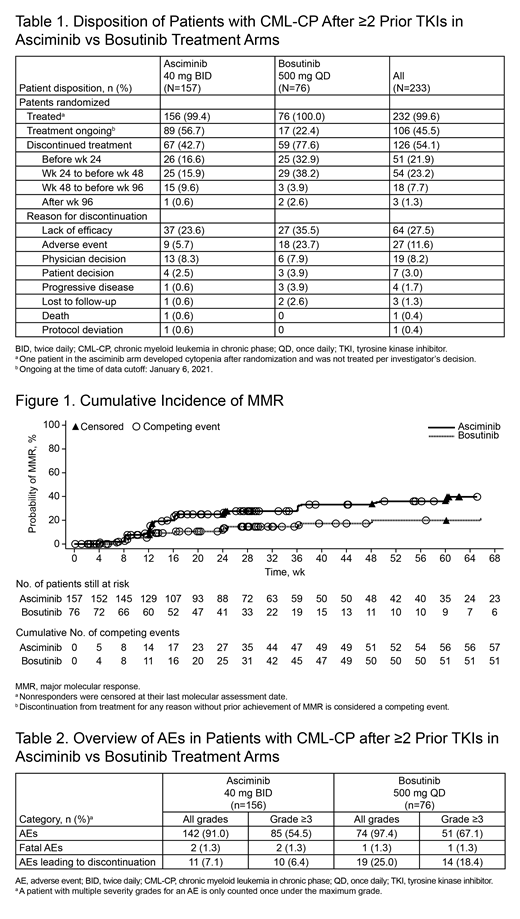
RESULTS: A total of 233 pts were randomized to receive either asciminib (n=157) or BOS (n=76). At cutoff, all randomized pts had completed their wk 48 visit or had discontinued earlier. Treatment was ongoing in 89 (56.7%) and 17 (22.4%) pts on asciminib and BOS, respectively; the most common reason for treatment discontinuation was lack of efficacy in 37 (23.6%) and 27 (35.5%) pts, respectively (Table 1).
By wk 48, the cumulative incidence of MMR was 33.2% with asciminib and 18.6% with BOS, showing that the difference between the 2 treatment arms observed by wk 24 in the primary analysis was maintained with longer follow-up (Figure 1). The cumulative incidence of BCR-ABL1IS ≤1% by wk 48 in patients without this level of response at baseline was 50.8% with asciminib and 33.7% with BOS. The difference in deep molecular responses (MRs) favoring asciminib vs BOS persisted by wk 48: MR 4 (BCR-ABL1IS ≤0.01%) and MR 4.5 (BCR-ABL1IS ≤0.0032%) rates were 14.0% and 9.6% with asciminib and 6.6% and 2.6% with BOS, respectively.
With a longer duration of exposure in the asciminib arm, the safety and tolerability profile in the current analysis remains similar to that at the primary analysis. Median duration of exposure was 67.1 wk (range, 0.1-162.1 wk) for asciminib and 29.7 wk (range, 1.0-149.3 wk) for BOS. By the cutoff date, 91.0% of pts on asciminib and 97.4% of pts on BOS reported ≥1 all-grade AE; 54.5% and 67.1% of pts, respectively, reported ≥1 grade ≥3 AE. No additional fatal events were reported since the primary analysis. Fewer pts in the asciminib (7.1%) than BOS (25.0%) arm experienced AEs leading to treatment discontinuation (Table 2). The most common AEs leading to treatment discontinuation included thrombocytopenia (3.2%) and neutropenia (2.6%) in the asciminib arm and increased alanine aminotransferase (5.3%) and neutropenia (3.9%) in the BOS arm.
CONCLUSIONS: Resistant/intolerant CML-CP after 2 lines of TKI treatment remains BCR-ABL1 dependent. The novel STAMP inhibitor asciminib demonstrates continued superior efficacy and a limited adverse event profile; myelosuppression, while more prominent, appears to be early and disease related. Secondary resistance based on loss of MMR is rare. Overall, after a median follow-up of 19.2 months, the positive benefit-risk profile of asciminib vs BOS continues to support the use of asciminib as a new therapy in this heavily pretreated pt population.
This study is sponsored by Novartis.
Mauro: Sun Pharma / SPARC: Research Funding; Pfizer: Consultancy; Bristol Myers Squibb: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Takeda: Consultancy. Minami: Takeda: Honoraria; CMIC: Research Funding; Astellas: Honoraria; Ono: Research Funding; Pfizer Japan Inc.: Honoraria; Novartis Pharma KK: Honoraria; Bristol-Myers Squibb Company: Honoraria. Rea: Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Incyte: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees. Hochhaus: Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; Bristol-Myers Squibb: Research Funding; Pfizer: Research Funding; Incyte: Research Funding. Lomaia: Novartis: Honoraria; Pfizer: Honoraria; BMS: Honoraria; Pharmstandard: Honoraria. Voloshin: Abbvie: Consultancy, Speakers Bureau; Novartis: Consultancy, Speakers Bureau; Astra Zeneca: Consultancy, Speakers Bureau; Pfizer: Consultancy; Biacad: Consultancy, Speakers Bureau. Turkina: Pharmstandart: Speakers Bureau; Novartis Pharma: Speakers Bureau; Bristol Myers Squibb: Speakers Bureau; Pfizer: Speakers Bureau. Kim: Novartis: Research Funding; BMS: Research Funding; Pfizer: Research Funding; ILYANG: Research Funding; Takeda: Research Funding. Apperley: Bristol Myers Squibb, Novartis: Honoraria, Speakers Bureau; Incyte, Pfizer: Honoraria, Research Funding, Speakers Bureau. Cortes: Sun Pharma: Consultancy, Research Funding; Bristol Myers Squibb, Daiichi Sankyo, Jazz Pharmaceuticals, Astellas, Novartis, Pfizer, Takeda, BioPath Holdings, Incyte: Consultancy, Research Funding; Bio-Path Holdings, Inc.: Consultancy, Membership on an entity's Board of Directors or advisory committees; Pfizer: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Takeda: Consultancy, Research Funding. Fogliatto: AstraZeneca: Speakers Bureau. Kim: Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Honoraria, Research Funding; Paladin: Honoraria, Research Funding; Bristol-Meier Squibb: Research Funding. le Coutre: Pfizer: Honoraria; Novartis: Honoraria; Incyte: Honoraria; Bristol Myers Squibb: Honoraria. Saussele: Novartis: Honoraria, Research Funding; BMS: Honoraria, Research Funding; Incyte: Honoraria, Research Funding; Pfizer: Honoraria; Roche: Honoraria. Hughes: Novartis: Honoraria, Research Funding; BMS: Honoraria, Research Funding; Incyte: Honoraria. Chaudhri: Abbvie: Honoraria; Novartis: Honoraria; Astra Zeneca: Honoraria. Chee: Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees. Garcia Gutierrez: Pfizer: Consultancy, Honoraria, Research Funding; Incyte: Consultancy, Honoraria, Research Funding; BMS: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding. Sasaki: Daiichi-Sankyo: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Research Funding. Kapoor: Novartis: Current Employment, Current equity holder in publicly-traded company. Allepuz: Novartis: Current Employment, Current equity holder in publicly-traded company. Quenet: Novartis: Current Employment. Bédoucha: Novartis: Current Employment. Boquimpani: Pinth Pharma: Speakers Bureau; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Jansen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal